7 minutes
1315 words
Is Mild Sleep Apnea Dangerous?
Catharine Nixon
January 28, 2023
Have you been diagnosed with mild sleep apnea and are wondering what it means for you?
Or, perhaps you suspect you might have sleep apnea but your signs and symptoms seem mild so you’re wondering whether it’s worth getting tested?
Let’s look at the diagnosis of mild sleep apnea and what that means for your health treatment options.
Sleep apnea severities explained – mild, moderate or severe?
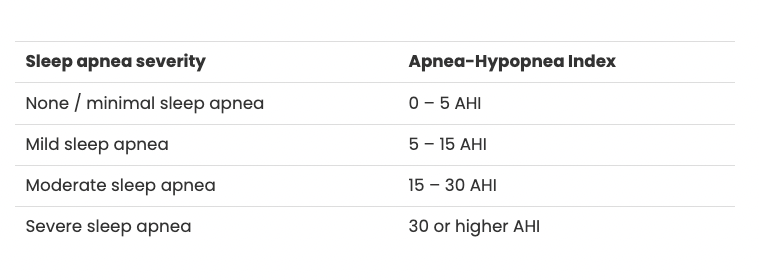
Mild sleep apnea is defined as having an AHI of between 5 and 15 per hour.
Back up! What is an AHI?
An AHI is short for ‘Apnea-Hypopnea Index’. It’s a way of putting a number on how severe your sleep apnea is. The number is worked out by adding up the number of apneas (pauses in breathing) and the number of hypopneas (shallow breathing episodes) that happen in an average hour of sleep.
During a sleeping test, the numbers of apneas and hyponeas are added up, then averaged out across the number of hours you slept for.
So, say your AHI was recorded at 10. That means that, on the night you were tested, you had either an apnea (breathing pause) or a hypopnea (shallow breathing) an average of 10 times per hour.
What is considered mild sleep apnea? The generally accepted levels of sleep apnea are:
Sleep apnea severity Apnea-Hypopnea Index
Now you know what an AHI is, you can see why sleep apnea is a big deal. Imagine stopping breathing or breathing very shallowly 10 times in an hour while awake? Having your breathing pause while you’re asleep might mean you’re less aware of it but it’s clearly not good news for you or your long term health.
AHI is an important measure for diagnosis, treatment and research purposes but there isn’t always an absolute connection between a higher AHI and greater day-to-day impacts of sleep apnea.
Someone with a lower AHI might find themselves dangerously sleepy, whereas another person with a higher AHI might be managing relatively well.
And, we are gradually learning that sleep apnea presents differently in women as compared with men (you can read more about this in our article titled Men and Women Sleep Apnea Signs and Differences).
There’s also evidence that sleep apnea tends to get worse over time (one study showed that half of mild patients progressed from mild sleep apnea to moderate or severe over four years).
So, unfortunately, having mild sleep apnea now may well mean that this will progress to moderate or severe sleep apnea in the months or years to come. Some of this worsening is linked to gaining weight but some of it seems to simply be because of time.
So, even if your AHI is in the mild range, your life might be significantly affected. And that means your sleep apnea is worth testing and treating.
What are the symptoms of mild sleep apnea?
Much of the research on sleep apnea is focussed on more severe forms of the disease. That’s understandable given the health risks associated with moderate and severe sleep apnea. But this can result in an underestimation of the risks associated with symptoms of mild sleep apnea.
Mild sleep apnea can result in daytime tiredness, poor concentration, clumsiness, depressed mood and insomnia, which adds up to a poor quality of life. And, all that sleepiness can lead to accidents, whether at home, at work or while driving.
Sleep apnea impacts other parts of your body. Leaving sleep apnea untreated can lead to other conditions like high blood pressure, heart attack, stroke, diabetes and depression.
Most of this research has been looking at people with more severe sleep apnea however there’s growing interest in the negative consequences of mild sleep apnea. For example, research in 2020 showed a link between mild OSA and high blood pressure.
There’s even evidence that people with sleep apnea have a high risk of death, especially when untreated. For those with mild sleep apnea, life expectancy data is not clear but there’s no question that mild sleep apnea is not good for your health.
Is treatment worth it for mild sleep apnea?
Lifestyle changes can make a big impact on sleep apnea. Losing weight, reducing alcohol consumption, treating any allergies, and sleeping on your side rather than your back can cure sleep apnea.
The good news for those with a diagnosis of mild sleep apnea is that these lifestyle changes are more likely to make a positive difference in a shorter period of time.
If lifestyle changes are not working, or not possible for you, then looking at other treatments is indicated, even if your sleep apnea is classified as mild.
The ‘gold standard’ treatment for sleep apnea is CPAP, or Continuous Positive Airway Pressure. A pump maintains a flow of air into your nose via a mask, which works to keep your airway open as you sleep.
CPAP can prevent apneas and therefore stop any broader negative consequences of sleep apnea. But it is not a complete cure. That’s because, if you stop using your CPAP machine at night, your symptoms will immediately return (unless you’ve combined CPAP use with lifestyle changes).
CPAP can work for sleep apnea mild symptoms, just like it does for moderate or severe forms of the condition. For example, research published in The Lancet in 2020 showed that people with mild sleep apnea who used a CPAP machine for three months reported improved quality of life.
Another treatment for sleep apnea is an oral appliance (which also go by the names of mandibular advancement splint or device). The idea is that you wear a mouthguard-like splint over your teeth that holds your jaw forward – and therefore your airway more open – as you sleep.
Other newer treatments are worth considering and we’re always hopeful of new devices becoming available soon!
Oral appliances don’t usually work well enough for people with severe sleep apnea but they are recommended for people with mild to moderate sleep apnea.
In summary
Mild sleep apnea is a recognised condition that can affect your daytime function and overall health as well as disrupting your night’s sleep. Lifestyle changes can cure mild sleep apnea and treatments such as CPAP can help manage the negative effects.
If left undiagnosed and untreated, mild sleep apnea can worsen and you’ll be unaware of the risks associated with the condition.
Mild sleep apnea is worth taking seriously. Sleep testing is recommended if you have any concerns about your quality of sleep. Read our article to find the best testing option for you.
References
Bouloukaki, I et al. (2020), Mild obstructive sleep apnea increases hypertension risk, challenging traditional severity classification. Journal of Clinical Sleep Medicine.
https://jcsm.aasm.org/doi/10.5664/jcsm.8354
Sahlman, J., Pukkila, M., Seppä, J. and Tuomilehto, H. (2007), Evolution of Mild Obstructive Sleep Apnea after Different Treatments. The Laryngoscope, 117: 1107-1111. https://doi.org/10.1097/MLG.0b013e3180514d08
Berger, R. Berger, A. Oksenberg (2009), Progression of snoring and obstructive sleep apnoea: the role of increasing weight and time. European Respiratory Journal 2009 33: 338-345; DOI: 10.1183/09031936.00075408
https://erj.ersjournals.com/content/33/2/338.short
Wimms, AJ et al (2020). Continuous positive airway pressure versus standard care for the treatment of people with mild obstructive sleep apnoea (MERGE): a multicentre, randomised controlled trial. The Lancet, 8(4): 349-358.
https://www.sciencedirect.com/science/article/abs/pii/S2213260019304023
McNicholas, WT et al (2020), Active management of mild obstructive sleep apnoea: the evidence grows. The Lancet Respiratory Medicine, Volume 8, Issue 4, April 2020, Pages 322-323
https://www.sciencedirect.com/science/article/abs/pii/S2213260019304473
Sleep Health Foundation Fact sheet on oral appliances.
Treating mild sleep apnea: Should you consider a CPAP device? Harvard Health Blog. https://www.health.harvard.edu/blog/treating-mild-sleep-apnea-should-you-consider-a-cpap-device-2020061520154